Speed vs Certainty: Why “Fastest Match” Can Increase Collaboration Risk for NPs
📌 Key Takeaways:
Finding a collaborating physician quickly shouldn't mean accepting one who doesn't understand your practice, can't clarify state requirements, or disappears when you need guidance.
Speed Without Vetting Creates Three Critical Gaps: Specialty misalignment leaves you without meaningful clinical guidance, compliance ambiguity exposes your license to audit risk, and poor communication protocols leave you alone during urgent situations.
Fastest Match Services Optimize for Volume, Not Fit: When the business model prioritizes how many practitioners a physician can supervise rather than how well they understand behavioral health, medical aesthetics, or telehealth protocols, you're paying for a signature on paperwork instead of genuine oversight.
State Requirements Vary Too Much for Generic Templates: What passes for adequate chart review in one state creates immediate audit vulnerability in another, and controlled substance oversight expectations differ dramatically across jurisdictions—making state-specific compliance clarity non-negotiable.
A Structured One-Week Process Balances Speed with Safety: Targeted vetting calls, documented service-level agreements, specialty-matched collaborators, and clear backup coverage protocols prove you can move quickly without the gaps that plague 48-hour matching services.
Communication Expectations Determine Real-World Reliability: A two-hour response SLA for urgent clinical questions, defined channels for different situations, monthly touchpoints for proactive review, and explicit backup coverage separate functional collaborations from regulatory formalities.
Week-long vetting beats same-day risk.
Nurse practitioners and physician assistants launching or expanding independent practices—particularly in telehealth, behavioral health, urgent care, medical aesthetics, infusion therapy, and integrative medicine—will find a practical evaluation framework here, preparing them for the detailed implementation guidance that follows.
The pressure to launch quickly creates real temptation. When you're building an independent practice—whether it's telehealth psychiatry, a medical aesthetics clinic, or urgent care—finding a collaborating physician fast feels like the most urgent priority. Services promising "instant matches" or "same-day approvals" sound appealing when you're racing to see patients and generate revenue.
But speed without certainty creates a different kind of risk. A collaborating physician who doesn't understand your specialty can't provide meaningful oversight. One who's unclear about your state's chart review requirements or controlled substance protocols puts your license at risk. And a supervisor who's consistently unavailable when you need guidance undermines the entire purpose of the collaboration.
The good news? You don't have to choose between speed and quality. With the right vetting framework, you can secure a well-matched, compliant collaboration in about a week—without the compliance gaps and communication failures that plague "fastest match" arrangements.
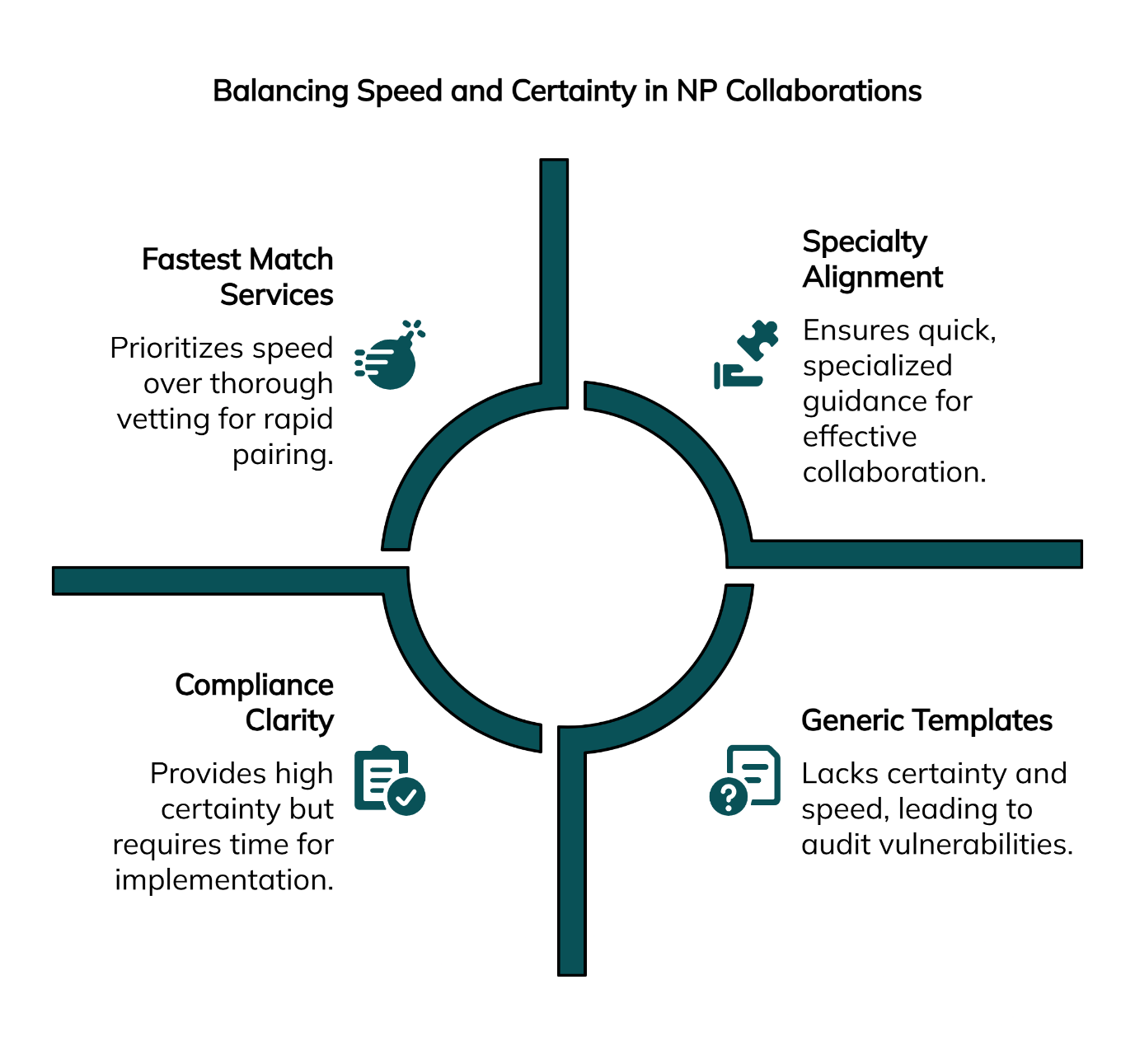
The Hidden Tradeoff: Speed vs Certainty in NP Collaborations
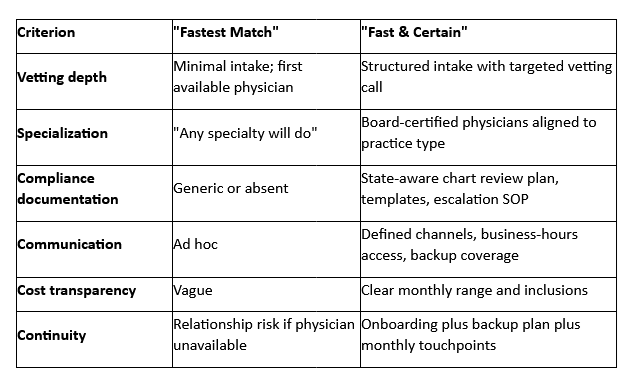
"Fastest match" services prioritize one metric above all others: how quickly they can pair you with any available physician. The business model is straightforward—maximize volume by minimizing the vetting process. While this approach gets you a signed agreement quickly, it often skips three foundational elements that determine whether a collaboration actually works.
Specialty alignment ensures your collaborating physician understands the clinical context of your practice. A family medicine physician supervising a psychiatric nurse practitioner faces a steep learning curve around psychopharmacology, risk assessment protocols, and behavioral health documentation standards. The mismatch doesn't just create clinical risk—it means you're essentially practicing without the specialized guidance that collaboration is designed to provide.
Compliance clarity means both parties understand exactly what your state requires and how you'll document it. Chart review cadence, scope of practice boundaries, prescriptive authority for controlled substances, and incident escalation pathways vary significantly across states. The National Council of State Boards of Nursing maintains comprehensive resources on state practice authority, but even with these guidelines, interpreting and implementing requirements correctly requires careful attention. Generic templates and vague oversight plans create audit vulnerabilities that surface only when a board investigation or payer audit occurs.
Operational responsiveness defines how you'll actually work together day-to-day. What communication channels will you use? What's the expected response time for clinical questions? Who covers when your collaborator is unavailable? These seemingly minor details determine whether you have dependable support or just a name on regulatory paperwork.
Where "Fastest Match" Goes Wrong
Mismatched Specialty Creates Clinical and Reputational Risk
Behavioral health practices face unique challenges when paired with generalist collaborators. Medication management for complex psychiatric conditions, suicide risk assessment, and involuntary commitment procedures require specialized knowledge. An internist who hasn't practiced psychiatry in years can't provide substantive guidance on managing treatment-resistant depression or navigating clozapine monitoring protocols.
Medical aesthetics and integrative medicine practices encounter similar problems. Cosmetic procedures, regenerative therapies, and integrative treatment protocols fall outside the comfort zone of many traditional primary care physicians. When complications arise—and in aesthetic medicine, they will—you need a collaborator who understands both the procedures and the risk management strategies specific to your field.
Telehealth adds another layer of complexity. Not all physicians are comfortable with virtual care delivery, and fewer still understand the nuances of prescribing controlled substances via telemedicine. State-specific telehealth regulations continue to evolve, and your collaborator needs current knowledge of these requirements to provide meaningful oversight.
Compliance Ambiguity Across States
State collaboration and supervision rules differ substantially in scope, documentation requirements, and oversight intensity. Some states mandate weekly chart reviews; others specify monthly or quarterly. The definition of "chart review" itself varies—some states accept retrospective reviews, while others require real-time or near-real-time oversight for certain practice types.
The American Association of Nurse Practitioners provides state-by-state practice environment resources that help clarify these requirements, while the Federation of State Medical Boards offers guidance on physician oversight obligations. Even with these authoritative resources, translating general guidelines into specific practice workflows requires careful attention to your state's unique requirements.
Controlled substance prescribing represents a particularly high-risk area. DEA registration, state monitoring program requirements, prescription limits, and documentation standards all demand precise understanding. A collaborator who provides only vague guidance—"just follow DEA rules"—leaves you exposed if an audit reveals documentation gaps or prescribing pattern concerns.
Documentation standards matter immensely. Board investigations often hinge on whether you can demonstrate appropriate oversight. Generic forms and templates that don't address your state's specific requirements create vulnerability. You need documented evidence of regular chart reviews, clinical consultations, quality improvement activities, and scope-of-practice discussions.
Poor Availability and Support Workflows
Consider the scenario: It's 2 PM on a Wednesday, and you have a patient experiencing unexpected medication side effects. You need clinical guidance within the hour to adjust the treatment plan safely. You text your collaborating physician, as discussed during onboarding. Four hours later, you're still waiting for a response.
This isn't a hypothetical edge case—it's a common pattern with low-cost, high-volume collaboration services. When physicians supervise dozens or hundreds of practitioners simultaneously, individual responsiveness suffers. If your agreement doesn't specify response timeframes, communication channels, and backup coverage, you're left managing clinical uncertainty alone.
Business hours availability creates another gap. If your practice operates evenings or weekends—common for urgent care and telehealth—and your collaborator is only available Tuesday through Thursday, 9 to 5, the timing mismatch creates obvious problems. Sample chart reviews scheduled at the collaborator's convenience, with no input from you about which cases would benefit most from discussion, miss opportunities for meaningful clinical guidance.
Get a free quote to discuss your specific practice needs and timeline.
A Safer Framework to Evaluate a Collaborating Physician—Fast
Specialty Fit in Five Questions
Start your vetting conversation with questions that reveal whether the physician genuinely understands your practice model:
What patient populations have you supervised in this specialty?
Listen for specific examples that match your practice type. A psychiatrist who has supervised NPs in outpatient behavioral health settings understands the clinical patterns, documentation requirements, and risk management strategies relevant to your work.
What procedures or treatment modalities are you comfortable overseeing?
For medical aesthetics, this means injectable procedures, laser treatments, and chemical peels. For integrative medicine, it includes nutritional therapies, IV infusions, and regenerative treatments. Generic answers like "I'm comfortable with anything within your scope" signal insufficient specialty knowledge.
How do you stay current in this specialty area?
Collaborators who attend relevant continuing education, read specialty journals, or participate in professional organizations bring more value than those who rely solely on decades-old training.
What telemedicine experience do you have?
If your practice operates virtually, your collaborator needs practical understanding of remote patient assessment, electronic prescribing workflows, and telehealth-specific documentation requirements.
Can you describe a challenging clinical situation you've helped a supervisee navigate?
Concrete examples demonstrate problem-solving ability and give you insight into the collaborator's communication style and clinical judgment.
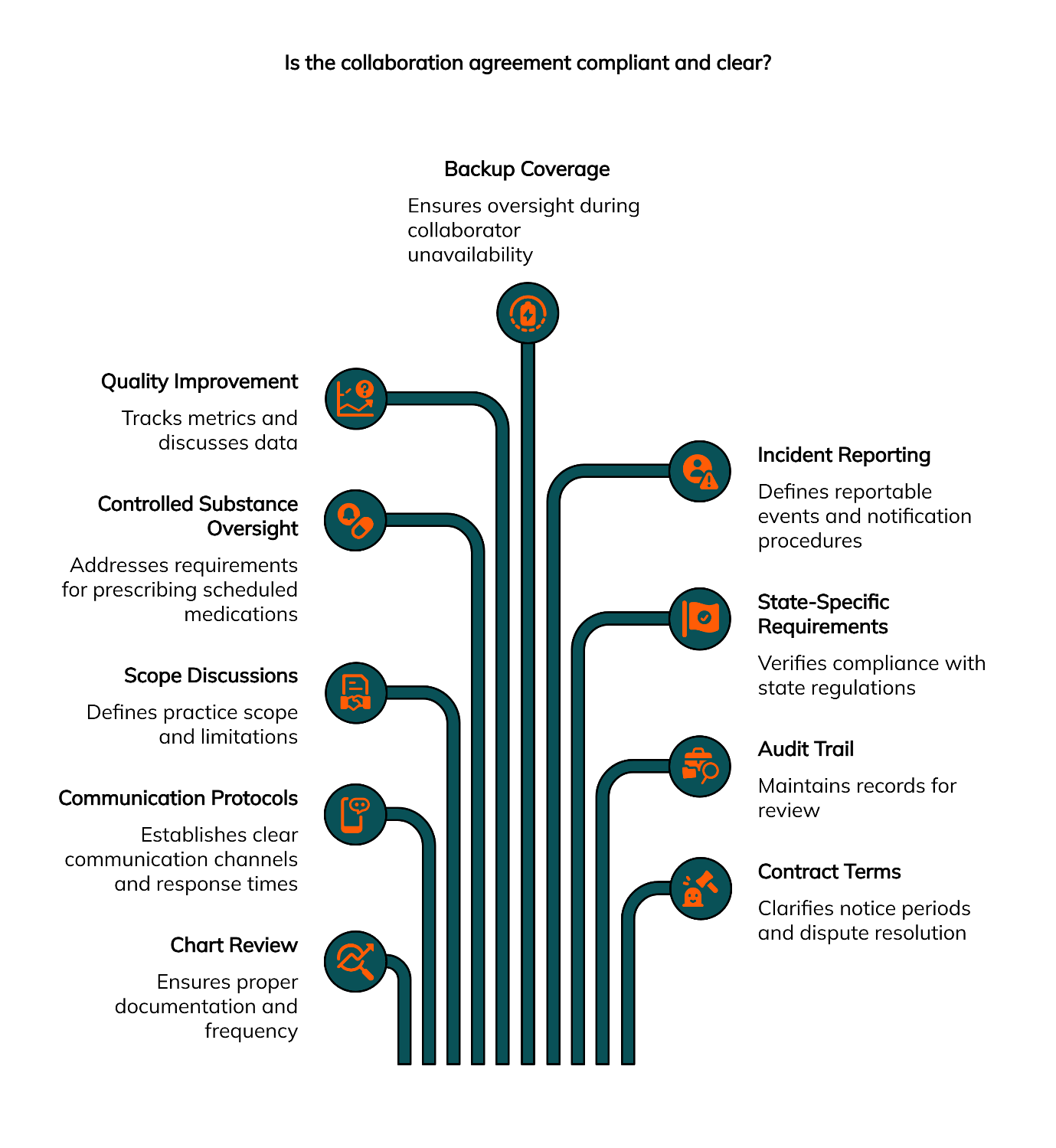
Compliance Certainty Checklist
Before finalizing any collaboration agreement, verify these elements are clearly defined:
Chart review schedule and methodology: How many charts? How often? What documentation will the physician provide?
Communication protocols: Which channels (text/phone/Zoom)? Expected response times during business hours? After-hours escalation pathways?
Scope discussions: How will you document your scope of practice and any limitations specific to your state or practice setting?
Controlled substance oversight: If applicable, what additional documentation or consultation requirements apply to prescribing scheduled medications?
Quality improvement activities: What metrics will you track together? How often will you discuss quality and safety data?
Backup coverage: Who provides oversight when your primary collaborator is unavailable? How is this transition communicated and documented?
Incident reporting: What constitutes a reportable event? How quickly must you notify your collaborator? What follow-up documentation is required?
State-specific requirements: Has the collaborator reviewed your state's current regulations? Can they cite specific statutes that govern your collaboration?
Audit trail: How will you maintain records of all oversight activities for board or payer review?
Contract terms: What's the notice period for either party? How are disputes resolved? What happens if you need to change collaborators?
Service-Level Signals
Professional collaboration services—whether individual physicians or networks—should clearly articulate their service-level agreements. Response time expectations during business hours should be specified in hours, not days. If they promise text/phone/Zoom access, ask for specific examples of how this works in practice.
Monthly touchpoints matter more than you might expect. Even when your practice is running smoothly, regular check-ins allow you to discuss challenging cases, review quality metrics, and address scope questions before they become urgent. Collaborators who offer only "as-needed" support often interpret that to mean "rarely."
Backup coverage deserves explicit discussion. Vacations, illnesses, and personal emergencies affect physicians just as they affect everyone else. If your collaborator becomes unavailable without notice and no backup system exists, you're left in a precarious position—unable to practice but still responsible for patient care.
Comparison: Fastest Match vs Fast and Certain
Explore our services to see practice types we support.
How Physician Collaborators Balances Speed and Certainty
Building a network of board-certified physicians across Internal Medicine, Family Medicine, Emergency Medicine, and Psychiatry allows us to match practitioners with collaborators who genuinely understand their specialty. When a behavioral health NP contacts us, we connect them with psychiatrists who have supervised similar practices. Medical aesthetics practitioners work with physicians familiar with cosmetic procedures and associated risk management.
The one-week timeline reflects a structured process, not corner-cutting. Initial intake captures your practice type, patient population, state requirements, and specific needs. Within 24–48 hours, we identify potential matches based on specialty alignment and availability. Vetting calls happen over the next few days, allowing you to assess clinical fit and communication style. By day five, you're reviewing a collaboration agreement with clear documentation of oversight protocols, communication channels, and compliance requirements.
This timeline works because the vetting happens upfront rather than after you've already committed. If the first match isn't quite right—perhaps the communication style doesn't click, or their availability doesn't align with your schedule—we identify an alternative before you sign anything.
We support diverse practice models: general medicine, behavioral health, telemedicine, urgent care, infusion therapy, integrative medicine, and medical aesthetics. Each practice type brings unique oversight requirements, and collaborators in our network understand these distinctions. A physician supervising an infusion therapy practice knows to focus on patient selection criteria, adverse reaction protocols, and billing documentation. One working with a med spa understands aesthetic complications, patient consent processes, and outcome documentation.
Geographic coverage spans many states, with particularly strong networks in New York, New Jersey, and Pennsylvania. State-specific regulations vary substantially—New York's collaboration requirements differ from Pennsylvania's practice agreements, which differ from New Jersey's collaborative practice structures. Collaborators familiar with your state's requirements reduce compliance risk significantly. Check our states page for current coverage, and review our detailed guides for New York, New Jersey, and Pennsylvania if you practice in those regions.
Implementation Guide: Replace "Instant Yes" with "Quality Fast"
Twenty-Minute Vetting Call Script
Structure your initial conversation with any potential collaborator around these five areas:
Specialty alignment discussion: "Can you walk me through your experience supervising [behavioral health/aesthetics/urgent care/integrative medicine] practitioners? What patient populations did they serve? What were the most common clinical questions that came up?"
Listen for concrete examples rather than generic assurances. A psychiatrist who supervised NPs in community mental health settings will describe specific scenarios—managing treatment-resistant depression, navigating involuntary commitment procedures, or adjusting medications for patients with co-occurring substance use disorders.
Oversight cadence and documentation: "What does your standard chart review process look like? How many charts do you review per month, and what documentation do you provide? Can you share a sample of your review template?"
Quality collaborators have clear answers and readily share examples. Vague responses—"We'll figure it out as we go"—or reluctance to show documentation templates are concerning signals.
Availability and communication protocol: "What channels do you prefer for clinical questions—text, phone, Zoom? During business hours, what's your typical response time? How do you handle coverage when you're unavailable?"
Specific answers indicate someone who has thought through the practical workflow. "I respond to texts within two hours during business hours, and I have a colleague who covers when I'm out of town" demonstrates more reliability than "Just reach out whenever you need me."
Escalation pathways and backup coverage: "If I encounter a clinical situation that requires immediate consultation—a potential medication interaction I'm concerned about, or a patient safety issue—what's the escalation process? Who should I contact if you're unreachable?"
Every practice encounters urgent situations occasionally. Collaborators who have thought through backup systems and escalation procedures demonstrate operational maturity.
Telemedicine, EMR familiarity, and security posture: If your practice operates virtually, "What telemedicine platforms have you used? Are you comfortable with electronic prescribing for controlled substances where state law permits? How do you manage HIPAA-compliant communication?"
Telemedicine expertise varies widely among physicians. Those who understand virtual care delivery, electronic health record integration, and secure communication platforms bring more value to telehealth practices.
Red flags to watch for during vetting: Vague answers on documentation suggest someone who hasn't established systematic processes. Claims that "any specialty will do" indicate lack of understanding about clinical distinctions that matter. Unclear coverage plans or backup arrangements mean you'll be on your own during absences. Unwillingness to share sample standard operating procedures, chart review templates, or communication protocols suggests either inexperience or reluctance to commit to defined workflows.
Documentation Pack for Onboarding
Once you've selected a collaborator, assemble these documents before your first day of practice together:
Chart review cadence document: Specifies how many charts you'll submit monthly (often a percentage of total patient encounters or a fixed number), what timeframe the physician has to complete the review, and what documentation format they'll provide. Include whether reviews are retrospective or near-real-time, and whether certain case types require immediate review.
Communication plan with SLA: Lists approved communication channels (text for brief questions, phone calls for more complex discussions, scheduled Zoom conferences for in-depth case review). Specifies expected response times—many collaborations use a two-hour SLA for urgent clinical questions during business hours. Documents after-hours protocols and emergency escalation pathways.
Scope notes: Outlines your scope of practice as defined by your state's regulations, any voluntary limitations specific to your practice setting, and procedures or situations that require collaborator consultation before proceeding. This document evolves as your practice grows and your scope expands.
Incident escalation standard operating procedure: Defines what constitutes a reportable incident (adverse drug reactions, patient safety events, scope-of-practice questions with legal implications), notification timeframes, and follow-up documentation requirements. Clear escalation procedures protect both parties and ensure appropriate response to serious situations.
One-Week Launch Checklist
Days 1–2: Intake, needs analysis, shortlist by specialty and state
Initial consultation captures essential information: practice type, specialty focus, patient demographics, planned procedures or services, geographic location, and state-specific requirements. The intake process should identify any unique aspects of your practice—such as serving a specialized population, using particular treatment modalities, or operating with specific scheduling constraints. This information drives the shortlist development, narrowing potential collaborators to those whose experience, specialty background, and availability align with your needs.
Days 3–4: Vetting calls, select finalist, draft agreement
Schedule calls with two or three potential matches to allow comparison. Use the vetting script described earlier to assess clinical fit, communication style, and operational reliability. After these conversations, select the collaborator whose specialty expertise, communication approach, and availability best match your practice requirements. Agreement drafting begins once you've identified your preferred partner, incorporating the specific oversight protocols, documentation requirements, and service-level commitments discussed during vetting.
Day 5: Compliance pack sign-off, EMR access plan, kickoff call
Finalize the documentation pack described above, ensuring all compliance requirements for your state are clearly addressed. If your collaborator will access your electronic medical record system for chart reviews, complete necessary access requests and security protocols this day. The kickoff call establishes working rhythms—setting initial chart review submissions, scheduling your first monthly conference, and confirming communication channels are functioning properly.
Days 6–7: First-week touchpoint and sample chart review
Submit your first small batch of charts for review, even if you've only seen a few patients. This early feedback loop helps calibrate documentation expectations and allows you to address any questions before they become patterns. The first-week touchpoint—a brief call or video conference—confirms everything is working smoothly and addresses any immediate concerns either party has about the arrangement.
Contact us to start your evaluation process.
Frequently Asked Questions
How fast is 'safe fast' for finding a collaborator?
Approximately one week is realistic when the vetting process addresses specialty fit, compliance requirements, and communication workflows. This timeline allows for meaningful evaluation without the gaps that create risk in same-day or 48-hour matching services. The key is that vetting happens before you commit, not after you've already signed an agreement.
What does collaboration actually include each month?
Standard collaboration includes sample chart review of an agreed-upon number of patient encounters, access to your collaborating physician via text, phone, or Zoom during business hours for clinical questions, and scheduled conferences when you need more in-depth discussion of complex cases or quality improvement initiatives. Response time expectations should be documented—typically within a few hours for urgent clinical questions during business hours.
What's the typical monthly cost range?
Monthly fees typically range from $500 to $1,250 depending on practice complexity, specialty requirements, and oversight intensity. Behavioral health practices with controlled substance prescribing, for example, often require more intensive oversight than general primary care. Medical aesthetics and integrative medicine practices may need specialized risk management guidance that affects pricing. Geographic location and state requirements also influence cost—states with more intensive supervision requirements typically command higher fees.
Do you support telemedicine and medical aesthetics practices?
Yes, along with general medicine, behavioral health, urgent care, infusion therapy, and integrative medicine. Each practice model brings distinct oversight needs. Telemedicine requires collaborators comfortable with virtual care delivery and electronic prescribing. Medical aesthetics demands understanding of cosmetic procedures and complication management. The matching process accounts for these specialization requirements.
Which states are available?
Current coverage includes many states across the U.S. The network continues to expand as regulatory environments evolve and practitioner needs grow. Visit our states page for the complete current list, and check state-specific pages for New York, New Jersey, and Pennsylvania for regional details.
Next Step: Choose Speed and Certainty
The fastest match isn't always the best match. When you're building an independent practice, the right collaborating physician becomes a genuine partner in your clinical success—someone who understands your specialty, knows your state's requirements, and provides dependable support when you need it.
The vetting framework outlined here helps you evaluate potential collaborators quickly without sacrificing the elements that actually matter: specialty alignment, compliance clarity, and operational responsiveness. A week spent on thorough evaluation prevents months of frustration with a mismatched collaboration that creates more risk than support.
Get a free quote to discuss your practice needs, timeline, and state requirements. Or explore our services to see the full range of practice types we support and check state availability to confirm coverage in your region. For answers to additional questions about collaboration expectations, visit our FAQ page.
Disclaimer: This article is for educational purposes and does not constitute legal advice. Collaboration requirements vary by state and payer. Always confirm current state rules and board guidance before implementing changes.
Our Editorial Process
Content is drafted by a collaborating physician with supervisory experience, medically reviewed by a senior collaborator for accuracy and completeness, and edited for clarity and compliance awareness. We verify monthly-cost ranges, oversight norms (e.g., sample chart reviews), and communication expectations against internal policies and current state-board guidance. We avoid competitor links and prioritize recognized authorities.
About Physician Collaborators
We connect nurse practitioners and physician assistants with board-certified collaborating physicians across Internal Medicine, Family Medicine, Emergency Medicine, and Psychiatry. Our network supports independent practices nationwide with specialty-matched oversight, compliance guidance, and responsive clinical support.