The Hidden Financial and Legal Risks of Informal Supervisory Agreements for NPs
📌 Key Takeaways
This investigative report reveals why informal "handshake deals" between nurse practitioners and physicians create hidden vulnerabilities that could destroy your practice and professional license.
The Trust Trap: What feels like a simple, relationship-based agreement actually exposes you to devastating financial disputes and sudden termination scenarios that formal contracts prevent through clear payment structures and notice periods.
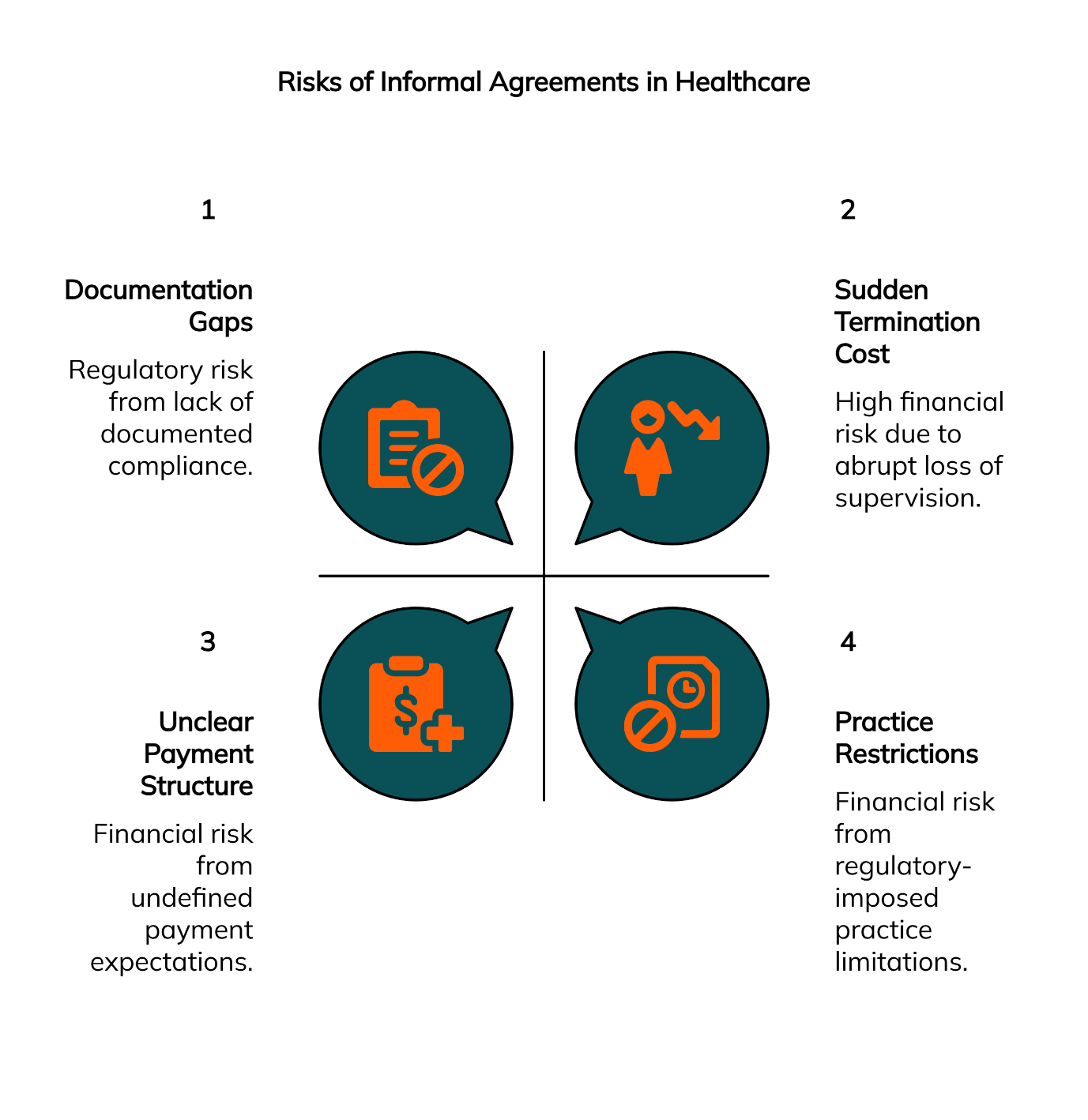
Your License Is at Stake: State licensing boards operate on documented proof, not personal relationships—informal agreements create "documentation gaps" that become critical vulnerabilities during audits, complaints, or regulatory inquiries.
The 5 Red Flags Checklist: Verbal-only terms, vague scope definitions, missing termination provisions, absent liability clarifications, and lack of emergency protocols serve as your early warning system for identifying dangerous supervisory arrangements.
The Regulatory Reality: Informal agreements often fail to meet specific state regulatory requirements for collaboration, leaving you without verifiable legal protection when you need it most—during patient complaints, audits, or board investigations.
From Anxiety to Confidence: True physician collaboration is a formal, strategic partnership designed for security and support, not an informal, risky paperwork exercise—choosing documentation over assumptions transforms anxious uncertainty into the confident security of a compliant practice.
The path to becoming a confident, established independent practice owner starts with this critical first step: recognizing that professional protection requires more than trust and good intentions—it demands the structural foundation that only formal, compliant agreements can provide.
The Lure of the 'Handshake Deal'
The conference room feels unusually quiet.
You're sitting across from a physician you've known for years through mutual colleagues. The conversation has been friendly, comfortable even. "Look," he says with a reassuring smile, "we don't need all that formal paperwork between us. We trust each other. A simple handshake agreement will work just fine for your collaboration needs."
It sounds so reasonable. So much simpler than navigating complex legal documents and regulatory requirements. The anxiety you've been carrying about establishing your independent practice seems to lift slightly. After all, isn't healthcare supposed to be built on trust and professional relationships?
But here's what's gnawing at you in the back of your mind: Am I sure this is enough to protect me?
This moment of uncertainty isn't unfounded. What feels like a straightforward, trust-based solution may actually expose you to significant legal and financial risks that could threaten everything you've worked to build. Welcome to our investigation into the hidden dangers lurking beneath informal supervisory agreements.
Key Terminology
Before we dive deeper, let's establish clear definitions for the critical concepts we'll be examining:
Collaborative Practice Agreement: A formal, written contract that defines the working relationship, scope of practice, and responsibilities between a nurse practitioner and supervising physician
Scope of Practice: The legally defined boundaries of what a nurse practitioner can do independently versus what requires physician oversight or collaboration
Regulatory Compliance: Meeting all state-specific legal requirements for nurse practitioner practice, including proper documentation and oversight structures
The Crime Scene: When Informal Agreements Lead to Financial Disaster
In our analysis of practitioner experiences, a disturbing pattern emerges. Informal agreements often fail to meet specific state regulatory requirements for collaboration. The financial consequences can be devastating.
The Unclear Payment Structure
One NP we encountered through our research learned this lesson the hard way. Her "handshake deal" with a collaborating physician seemed straightforward initially—$800 per month for chart reviews and consultation availability. But six months into the arrangement, the physician suddenly demanded additional compensation for what he claimed were "extra consultations."
Without a written agreement defining the scope of services, this practitioner found herself in an impossible position. Pay the additional fees and watch her practice margins evaporate, or risk losing her collaborative relationship entirely.
The fundamental problem is that verbal financial arrangements lack the specificity needed for sustainable business relationships. When expectations aren't clearly documented, both parties operate on assumptions that rarely align perfectly.
The Sudden Termination Cost
Perhaps even more dangerous is the scenario where an informal collaboration ends abruptly. 'Handshake deals' provide no verifiable legal protection for the NP in cases of patient complaints, audits, or board inquiries.
Consider what happens when a collaborating physician decides to retire, relocate, or simply discontinue the informal arrangement. Without contractual notice periods or transition provisions, you could find yourself without required supervision overnight. The cost of emergency practice closure while scrambling to find new collaboration can reach tens of thousands of dollars in lost revenue and administrative expenses.
"Without a formal contract defining roles and responsibilities, liability becomes a grey area that puts both parties at greater risk."
The Prime Suspect: Vague Terms and Your Professional License
Here's where the investigation takes a more serious turn. Your professional license represents years of education, training, and investment. It's not just your credential—it's your livelihood.
State licensing boards operate on documented evidence, not personal relationships or good intentions. When they conduct audits or investigate complaints, they require specific proof that you're operating within legally compliant supervisory arrangements.
An informal agreement creates what regulatory experts call "documentation gaps." These gaps become critical vulnerabilities during licensing inquiries. Board investigators don't accept explanations like "the doctor and I had an understanding." They need to see written protocols, defined scope of practice boundaries, and documented oversight processes.
Business Impact: The Regulatory Compliance Gap
From a practice management perspective, informal agreements create systemic operational risks. Vague or verbal financial arrangements in informal agreements are unstable and can lead to costly disputes or unexpected termination of the relationship.
The business implications extend beyond immediate financial concerns. When regulatory agencies identify compliance gaps, they can impose practice restrictions, require additional oversight periods, or in severe cases, suspend practice privileges entirely. The revenue impact of even temporary practice limitations can be devastating for independent practitioners.
Myth & Fact
Myth: "A friendly 'handshake deal' with a physician I know and trust is good enough."
Fact: Trust is essential, but it doesn't replace legal and regulatory requirements. State boards operate on documented proof, not personal relationships. A formal agreement protects both you and the trusted physician.
Case File: 5 Red Flags That Signal a Risky Agreement
True physician collaboration is a formal, strategic partnership designed for security and support, not an informal, risky paperwork exercise. Here's your investigative toolkit for identifying potentially dangerous supervisory arrangements:
Red Flag #1: Verbal-Only Terms
Any collaboration arrangement that exists solely through spoken agreements lacks the documentation required for regulatory compliance. Written terms provide legal protection and clarity for both parties.
Red Flag #2: Vague Scope Definitions
If the agreement doesn't clearly specify which cases require consultation, what constitutes appropriate independent practice, and when direct physician involvement is mandatory, you're operating in a regulatory gray area.
Red Flag #3: No Termination Provisions
Arrangements without defined notice periods, transition protocols, or continuity planning leave you vulnerable to sudden practice disruption.
Red Flag #4: Missing Liability Clarifications
Without explicit statements about professional liability coverage, indemnification, and responsibility allocation, both parties face increased legal exposure.
Red Flag #5: Absent Emergency Protocols
Collaborative agreements must include specific procedures for urgent consultations, after-hours coverage, and emergency decision-making authority.
These red flags serve as your early warning system. When you can confidently identify and avoid these warning signs, you're building the foundation for a secure, compliant practice that will serve you throughout your career.
Common Pitfalls to Avoid When Establishing Collaboration
Our research reveals several recurring mistakes that independent practitioners make during the collaboration setup process.
Failing to Verify Physician Credentials
Never assume that a physician's willingness to collaborate automatically indicates their qualifications to do so. Always verify current licensing, any disciplinary actions, and relevant specialty experience. State boards often require collaborating physicians to meet specific criteria that extend beyond basic medical licensure.
Ignoring State-Specific Clauses
Regulatory requirements vary significantly between states. A collaboration model that works perfectly in New York may not meet the specific documentation or oversight requirements mandated in Pennsylvania or New Jersey.
Not Planning for Contingencies
Most practitioners focus on establishing the initial relationship but fail to consider what happens when circumstances change. Physician retirement, illness, or practice changes can disrupt your collaboration suddenly. Formal agreements should always include succession planning and alternative coverage arrangements.
Expert Q&A
Question: What specific clauses must be in my agreement to be compliant?
Answer: According to the Physician Collaborators Insights Team, compliant agreements must include: defined scope of practice boundaries, specific chart review processes and timelines, clear emergency consultation protocols, explicit liability and indemnification terms, termination and transition procedures, and documentation of the collaborating physician's credentials and authority. The exact requirements vary by state, making professional guidance essential for ensuring full compliance.
What If...? Planning for a Sudden Loss of Supervision
Your concern about a physician backing out of an informal arrangement is not just valid—it's prudent professional planning. This scenario happens more frequently than many practitioners realize.
The anxiety you feel about this possibility reflects good business instincts. When collaboration depends entirely on one person's continued availability and goodwill, you're building your practice on an unstable foundation.
Here's your two-step protection plan:
Step 1: Establish Termination Protections Even in formal agreements, ensure you have adequate notice periods (typically 30-90 days) and transition assistance provisions. This gives you time to arrange alternative collaboration without practice disruption.
Step 2: Build Backup Systems Consider working with established collaborating physicians who maintain networks of qualified practitioners. This approach provides built-in redundancy and reduces your vulnerability to single-point-of-failure scenarios.
The goal isn't to eliminate all risk—that's impossible in any business relationship. Instead, you're creating manageable risk levels that allow you to maintain practice continuity even when circumstances change unexpectedly.
Technical Note
For implementation purposes, maintain digital copies of all collaboration documentation in secure, HIPAA-compliant storage systems. Cloud-based practice management platforms often include compliance tracking features that can help you monitor agreement renewals, credential expiration dates, and required documentation updates automatically.
A Question You Should Be Asking
The Unasked Question: "What is my supervising physician's actual legal responsibility if I'm sued, and how does an informal agreement impact that?"
Why It Matters: Without clear contractual definitions of liability and indemnification, you may discover too late that your informal collaboration provides less legal protection than you assumed. This uncertainty can become critical during malpractice claims or regulatory investigations.
The Expert Answer: Formal agreements explicitly define liability allocation, professional responsibility boundaries, and indemnification obligations. When these elements are left undefined in informal arrangements, courts and regulatory bodies must interpret the relationship based on limited evidence, often resulting in unfavorable determinations for both parties.
Case Closed: Securing Your Practice with a Formal Agreement
Our investigation reveals a clear pattern of evidence. Informal supervisory agreements consistently expose nurse practitioners to financial instability, regulatory compliance gaps, and professional license risks that formal arrangements effectively eliminate.
The temptation of the "handshake deal" is understandable. It promises simplicity in a world of complex regulations and legal requirements. But as we've documented throughout this investigation, that apparent simplicity masks serious vulnerabilities that can threaten your entire professional future.
Regulatory compliance prevents licensure actions. A formal collaborative practice agreement enables practice security. These aren't abstract legal concepts—they're practical protections that allow you to focus on patient care rather than constantly worrying about compliance gaps.
The transformation from anxious uncertainty to confident security begins with recognizing that true collaboration requires more than trust and good intentions. It demands the structural foundation that only formal, compliant agreements can provide.
Your journey toward becoming a confident, established independent practice owner starts with this critical first step: choosing security over convenience, documentation over assumptions, and professional protection over informal promises.
Ready to build the secure foundation your practice deserves? Contact Physician Collaborators today for a free consultation on establishing compliant, protective collaboration agreements.
This article provides general information about the risks of informal supervisory agreements for educational purposes. Individual circumstances vary significantly based on factors like state regulations, practice specialty, and specific operational requirements. For personalized guidance tailored to your practice's compliance needs, it is recommended to consult with a qualified professional.
Our Editorial Process
Our expert team uses AI tools to help organize and structure our initial drafts. Every piece is then extensively rewritten, fact-checked, and enriched with first-hand insights and experiences by expert humans on our Insights Team to ensure accuracy and clarity.
About the Physician Collaborators Insights Team
The Physician Collaborators Insights Team is our dedicated engine for synthesizing complex topics into clear, helpful guides. While our content is thoroughly reviewed for clarity and accuracy, it is for informational purposes and should not replace professional advice.