Why a Generalist Collaborator Is a Risk for Your Behavioral Health Practice
📌 Key Takeaways
The hidden risk in your behavioral health practice isn't non-compliance—it's the clinical and professional vulnerability that comes from specialty mismatch in physician collaboration.
The Compliance Myth: Having a signed collaborative agreement with any physician meets legal requirements, but specialty mismatch between a generalist collaborator and psychiatric practice creates measurable risks in clinical decision-making, professional defensibility, and regulatory scrutiny.
Three Critical Risk Areas: Complex psychopharmacology requires specialized knowledge of psychiatric drug interactions and emerging protocols; evolving behavioral health diagnostics demand expertise in trauma-informed care and cultural considerations; and malpractice insurers and state boards increasingly examine whether supervising physicians possess relevant expertise for the specialty care provided.
Real-World Vulnerability: When facing board inquiries or malpractice claims, the appropriateness of clinical oversight becomes central—communications with a psychiatric collaborator demonstrate specialty-appropriate decision-making, while generalist supervision often reveals consultation gaps that investigators interpret as inadequate oversight.
The Documentation Defense: Peace of mind comes from knowing your collaborating physician understands psychiatric care nuances, making clinical decisions more confident, documentation more precise, and creating a stronger professional defense during any regulatory review.
Investment vs. Expense Mindset: Choosing a specialist collaborator transforms you from a compliance-focused practitioner to a partnership-minded professional committed to excellence—positioning this decision as a foundational investment in patient safety, professional integrity, and long-term practice success.
True collaboration means clinical partnership that enhances patient safety and practitioner confidence, not just signing paperwork to meet legal minimums.
The Compliance Myth - When 'Good Enough' Isn't Good Enough
Picture this: You've built a thriving psychiatric practice. Your patients trust you. Your clinical skills are sharp. But late at night, a nagging question keeps surfacing—Is my family practice collaborator really qualified to oversee my specialized work?
You're not alone in this concern. Many behavioral health nurse practitioners find themselves in this exact position, having secured what appears to be a perfectly compliant collaborative agreement with a generalist physician. The paperwork is signed. The legal box is checked. Yet something feels fundamentally misaligned.
This isn't about questioning your collaborating physician's competence as a medical professional. It's about recognizing that psychiatric care operates in a specialized realm that demands equally specialized oversight. The difference between compliance on paper and clinical defensibility in practice can mean everything when your license and reputation are on the line.
What if there was a way to transform this lingering anxiety into confident, defensible practice standards?
The Investigation: Uncovering Hidden Clinical Gaps
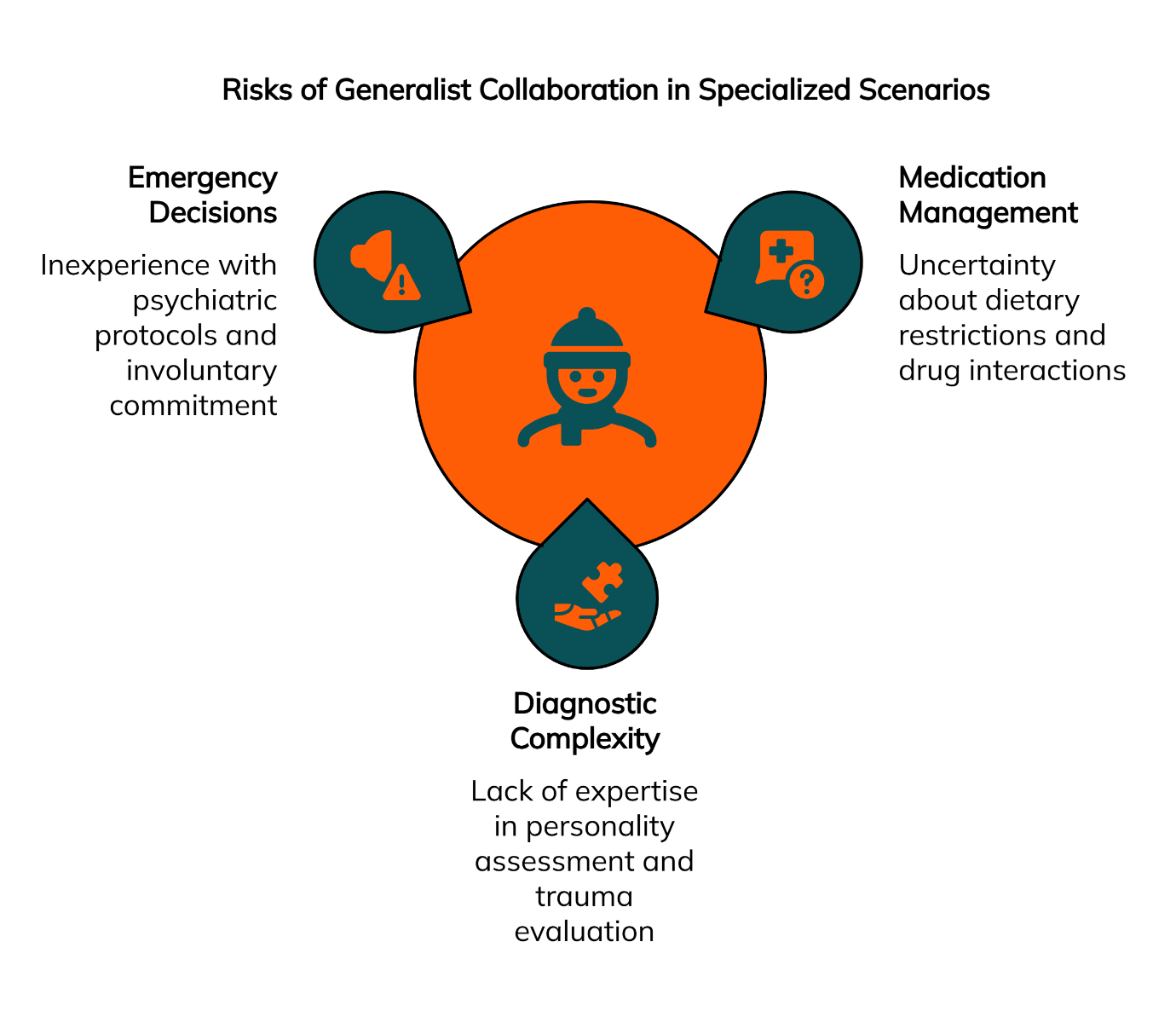
Like any thorough investigation, we need to examine the evidence. The reality facing psychiatric nurse practitioners today reveals three critical areas where generalist collaboration creates measurable risk
Risk #1: Complex Psychopharmacology and the Limits of Generalist Knowledge
Modern psychiatric pharmacology has evolved into a highly specialized field requiring deep, current expertise. Consider the complexity involved in managing a patient with bipolar disorder who's also dealing with substance use issues and metabolic concerns from antipsychotic medications.
A collaborating psychiatrist brings specialized knowledge of drug-drug interactions specific to psychiatric medications, understanding of genetic testing for medication metabolism, and awareness of emerging treatment protocols that generalist physicians simply don't encounter in their daily practice.
The American Journal of Psychiatry regularly publishes updates on psychiatric medication management that may not reach the generalist medical community for months or years. This knowledge gap isn't a reflection of professional inadequacy—it's a natural result of specialization in medicine.
Risk #2: Evolving Diagnostics and the Standard of Care in Behavioral Health
Psychiatric diagnostics have undergone significant evolution with advances in understanding trauma-informed care, cultural considerations in mental health, and the integration of social determinants into treatment planning. These nuances require continuous education and practical experience that generalist physicians rarely obtain.
Business Impact: Practices that align their oversight with their specialty focus may experience benefits in operational efficiency and clinical confidence. When collaborating physicians understand the unique documentation requirements, treatment protocols, and regulatory expectations of behavioral health, this alignment can reduce the administrative burden of explaining specialized procedures and create smoother workflows for complex cases.
The standard of care in behavioral health now encompasses not just symptom management but comprehensive assessment of trauma history, cultural factors, and social supports—areas where specialized training makes a critical difference in both patient outcomes and professional defensibility.
Risk #3: The Scrutiny of Malpractice Insurers and State Boards
Here's where the investigation reveals its most concerning findings. When malpractice claims or board inquiries occur, the appropriateness of clinical oversight becomes a central focus.
Technical Note: Some malpractice insurance carriers have begun incorporating risk assessment factors that include the appropriateness of clinical supervision for specialized practices. While policies vary significantly across insurers and states, claims reviewers increasingly examine whether the supervising physician's expertise aligns with the complexity of care provided, particularly in high-risk specialties like psychiatry.
In certain jurisdictions, state licensing boards are examining collaborative relationships more closely, looking beyond mere compliance to evaluate whether the collaboration meaningfully supports safe practice standards. However, this trend varies considerably by state, with some states granting nurse practitioners full practice authority and others maintaining different supervision requirements entirely.
Deep Dive: Understanding Specialty-Specific Clinical Nuance
The heart of this issue lies in understanding what "specialty-specific clinical nuance" actually means in behavioral health practice. This involves far more than basic medication knowledge or diagnostic criteria.
Psychiatric care requires understanding the interplay between medications and psychotherapy modalities, recognition of subtle medication side effects that can mimic psychiatric symptoms, and awareness of how psychiatric conditions present differently across diverse populations. These competencies develop through specialized training and ongoing practice within the field.
When a patient experiences breakthrough symptoms while on a complex medication regimen, the supervising physician needs immediate, intuitive understanding of the clinical landscape. A generalist, no matter how competent, must rely on consultation or research that delays critical decision-making.
Day-to-Day Application: Consider a typical scenario where a patient calls reporting concerning side effects from a recently adjusted mood stabilizer. A psychiatric specialist immediately recognizes whether this represents a dosing issue, drug interaction, or potentially serious adverse reaction, guiding appropriate triage decisions. This level of specialized knowledge directly impacts patient safety and clinical efficiency.
Red Flags: 3 Scenarios Where a Generalist Collaborator Creates Risk
Here are three real-world scenarios that demonstrate when generalist collaboration becomes professionally precarious:
The Complex Medication Management Case: A 35-year-old patient with treatment-resistant depression requires a specialized medication combination including an MAOI inhibitor. Your generalist collaborator expresses uncertainty about the dietary restrictions and drug interactions, requiring extensive consultation that delays treatment. During a subsequent malpractice review, questions arise about whether appropriate psychiatric expertise was available for this high-risk medication decision.
The Diagnostic Complexity Situation: You're treating a patient presenting with symptoms that could indicate bipolar disorder, borderline personality disorder, or trauma-related conditions. The diagnostic differentiation requires specialized expertise in personality assessment and trauma-informed evaluation. Your generalist collaborator, unfamiliar with these nuances, cannot provide meaningful clinical guidance, potentially compromising both patient care and your professional standing.
The Emergency Decision Scenario: A patient in crisis requires immediate hospitalization decisions involving psychiatric holds and medication management. Your generalist collaborator lacks experience with emergency psychiatric protocols and involuntary commitment procedures. During a board inquiry following the incident, investigators question whether appropriate psychiatric oversight was available for these critical decisions.
Each scenario illustrates how specialty mismatch creates both immediate clinical challenges and long-term professional vulnerability.
Key Terminology Box:
Collaborating Physician: A doctor who provides formal oversight and consultation for a Nurse Practitioner as required by state law
Standard of Care: The level of skill and diligence that a reasonably prudent healthcare provider in the same specialty would exercise under similar circumstances
Scope of Practice: The services that a qualified health professional is deemed competent to perform, and permitted to undertake – in keeping with the terms of their professional license
What If...? Planning for a Board Inquiry or Malpractice Claim
This question haunts many psychiatric nurse practitioners, and rightfully so. When regulatory scrutiny occurs, having appropriate specialty oversight becomes your strongest professional defense.
Board investigators and malpractice attorneys examine whether the supervising physician possessed relevant expertise to meaningfully oversee the care provided. A generalist's supervision of psychiatric care raises immediate questions about clinical appropriateness and adherence to specialty standards.
The documentation trail becomes crucial during these reviews. Communications between you and a psychiatric collaborator demonstrate specialty-appropriate oversight and decision-making. Conversations with a generalist often reveal the consultation gaps and knowledge limitations that investigators interpret as inadequate supervision.
Myth & Fact:
Myth: "As long as I have a signed collaborative agreement with any physician, I am legally protected."
Fact: "While a signature meets the basic requirement, state boards and malpractice carriers often look for substantive, specialty-appropriate collaboration during an inquiry. A mismatch can be viewed as a failure to ensure the highest standard of care."
Expert Q&A:
Question: "Can an internist or family medicine doctor supervise a psychiatric NP?"
Answer: "While some states may legally permit it, the best practice and the standard increasingly expected by malpractice insurers is for the collaborating physician's specialty to match the NP's practice area. For a behavioral health practice, this means a collaborating psychiatrist is the most appropriate and defensible choice."
The peace of mind that comes from appropriate specialty collaboration cannot be overstated. When you know your collaborating physician understands the nuances of your practice, clinical decisions become more confident, documentation becomes more precise, and professional anxiety diminishes significantly.
The Verdict: An Investment in Safety and Excellence
Our investigation reveals a clear conclusion: choosing a specialist collaborator isn't an expense—it's an essential investment in patient safety, professional integrity, and long-term practice success.
The evidence demonstrates that specialty mismatch in collaboration creates measurable risks across clinical, legal, and professional domains. While generalist collaboration may satisfy basic regulatory requirements, it falls short of the standard of care increasingly expected in today's healthcare environment.
"Compliance on paper is not the same as defensibility in practice."
This transformation from compliance thinking to partnership thinking positions you not just as a rule-follower, but as a practitioner committed to excellence. Five years from now, as you look back on building your respected behavioral health practice, this decision to prioritize appropriate specialty collaboration will stand as a foundational moment in your professional journey.
The path forward is clear. Your patients deserve psychiatric expertise in their care oversight. Your professional reputation demands it. Your future success depends on it.
Ready to make this critical investment in your practice's foundation? Book your free consultation to connect with experienced collaborating psychiatrists who understand the unique demands of behavioral health practice.
This article provides general information about the risks of a generalist collaborator for educational purposes. Individual circumstances vary significantly based on factors like your specific state regulations, the complexity of your patient population, and your malpractice insurance requirements. For personalized guidance tailored to your behavioral health practice's compliance and clinical oversight needs, it is recommended to consult with a qualified professional.
Our Editorial Process
Our expert team uses AI tools to help organize and structure our initial drafts. Every piece is then extensively rewritten, fact-checked, and enriched with first-hand insights and experiences by expert humans on our Insights Team to ensure accuracy and clarity.
About the Physician Collaborators Insights Team
The Physician Collaborators Insights Team is our dedicated engine for synthesizing complex topics into clear, helpful guides. While our content is thoroughly reviewed for clarity and accuracy, it is for informational purposes and should not replace professional advice.