Beyond Compliance: How the Right Collaborating Physician Accelerates Practice Growth
📌 Key Takeaways
Most independent nurse practitioners treat collaboration as paperwork, but that signature line represents untapped practice potential.
Specialty Alignment Compounds Over Time: A psychiatrist collaborator unlocks complex medication protocols and crisis pathways that a general practitioner simply cannot support, creating exponential service expansion over 12-24 months.
Response Speed Drives Revenue Retention: Text-accessible physician guidance during business hours transforms clinical uncertainty into same-day decisions, keeping patients in-house instead of referred out.
Audit-Proof Documentation Requires Real Oversight: Signature-only arrangements collapse under state board scrutiny when there's no documented chart review trail or accessible communication history.
Patient Location Governs Telehealth Compliance: Multi-state telehealth expansion fails without collaborators licensed where patients physically sit during visits, not where the NP practices from.
Retainer Models Buy Predictability, Not Transactions: Monthly partnerships averaging $500-$1,250 fund ongoing mentorship and systematic feedback rather than per-question billing that creates access barriers.
Growth-minded collaboration beats compliance-only arrangements through specialty expertise, documented oversight, and operational velocity. Independent nurse practitioners in reduced or restricted practice states will find this strategic framework here, preparing them for the detailed evaluation criteria and state-specific considerations that follow.
Opening an independent NP practice means navigating a complex regulatory landscape that varies significantly by state. In states with reduced or restricted practice authority, one requirement consistently appears: securing a collaborating physician. Many practitioners in these states view this as a legal formality—a signature to satisfy the board. But that mindset misses a crucial opportunity.
Think of your collaboration requirement like a building's foundation. Compliance gives you the concrete base that keeps your practice legally sound. That's essential, of course. But a quality collaborating physician provides something far more valuable: the framework that lets you build upward. With the right partner, that foundation supports expanded services, faster clinical decisions, and stronger market positioning.
Picture a behavioral health NP facing a common scenario. A patient presents with treatment-resistant depression and complex medication interactions. Without accessible specialist support, the options narrow to conservative treatment or external referral. With a psychiatrist collaborator available by text during business hours, that same NP can confidently adjust protocols, discuss nuanced approaches, and retain both the patient and the revenue. The difference isn't just clinical—it's operational and financial.
This guide explores how to evaluate potential collaborating physicians beyond their license and signature. The goal: finding a growth partner who accelerates your practice trajectory rather than simply checking a regulatory box.
What Does a Great Collaborator Actually Change in Your Practice?
A well-matched collaborating physician reduces clinical uncertainty, expands your service range, and speeds up safe decision-making. These aren't abstract benefits. They translate directly into practice capabilities that would otherwise remain out of reach.
Consider a telemedicine practice serving patients across multiple states. State regulations vary significantly, with the American Association of Nurse Practitioners classifying environments as full practice, reduced, or restricted based on collaboration requirements. A collaborator with multi-state licensure and telehealth experience doesn't just satisfy the rules—they provide guidance on state-specific scope variations, help navigate interstate prescribing complexities, and support confident expansion into new markets. That's the difference between cautious, limited operations and strategic growth.
For NPs offering specialized services like infusion therapy or integrative medicine, specialty-aligned oversight becomes even more critical. A general family medicine physician may meet the legal requirement but lacks the depth to mentor on complex protocols. The result: conservative treatment plans, hesitant service expansion, and missed revenue opportunities.
The 3 Ways a Collaborating Physician Drives Growth
1. Clinical Confidence for More Complex Cases
Access to specialty-aligned guidance means fewer external referrals and smarter clinical triage. When questions arise about dosing adjustments, unusual presentations, or treatment escalation, having a collaborator available via text, email, or phone during business hours transforms uncertainty into action. Monthly sample chart reviews—a standard component of structured collaboration—help identify patterns early and refine protocols systematically. Patients stay within your practice rather than being referred out. Your scope of comfortable practice expands month by month.
2. Reputation Lift and Payer Confidence
Quality collaborations signal to both patients and payers that your practice maintains high standards. During credentialing processes, insurance companies evaluate not just your credentials but your support structure. Board-certified physician oversight with documented chart reviews provides measurable quality assurance. This isn't marketing language—it's documentation that speeds approvals and strengthens retention. You can credibly position your practice as NP-led with physician collaboration for quality assurance, which addresses concerns from both referral sources and prospective patients.
3. Operational Speed and Reduced Decision Friction
Clinical questions don't arrive on convenient schedules. They surface during patient visits, after hours, or when reviewing weekend labs. When your collaborator responds within hours rather than days—and when escalation to a Zoom consultation for complex cases is standard rather than exceptional—your practice velocity increases. Research on professional mentorship confirms that accessible guidance from experienced advisors accelerates decision-making and reduces uncertainty in complex professional roles. Problems get resolved quickly. Patient satisfaction improves. Your own cognitive load decreases.
Specialty Match Over Generalist: The Compounding Advantage
Regulatory language often uses neutral terms like "collaborating physician" without specifying specialty requirements. This creates a temptation to prioritize convenience or cost over clinical alignment. That's a strategic error with compounding consequences.
A psychiatric NP working with a family medicine collaborator faces systematic limitations. The generalist may satisfy state board requirements but lacks depth on psychopharmacology nuances, complex medication interactions, or emerging treatment protocols. Every clinical question becomes a teaching moment rather than a collaborative discussion. Growth stalls because the oversight structure can't support service expansion.
Contrast that with a psychiatric NP partnered with a board-certified psychiatrist. Conversations shift from basic approval-seeking to strategic problem-solving. The NP gains confidence tackling more complex presentations. The practice can credibly market specialized services because the oversight truly supports them. This pattern holds across specialties: when clinical expertise aligns between NP and collaborating physician, both clinical safety and practice growth potential increase. Practitioners consistently report that specialty mismatches create unnecessary constraints on service expansion and confidence in complex case management.
The Growth Partner Evaluation Matrix
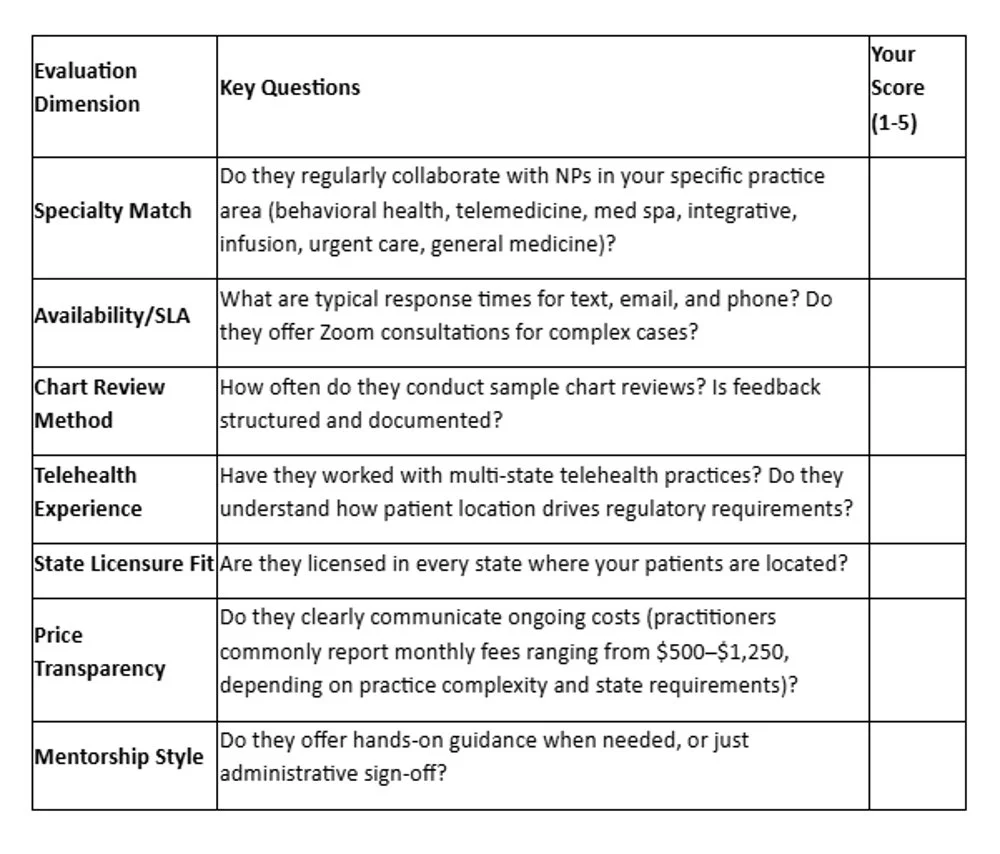
Not all collaborating physicians function as true partners. Use these seven criteria to evaluate potential matches, scoring each on a 1-5 scale:
Prioritize partners scoring 4 or higher on Specialty Match, Availability/SLA, and State Licensure Fit. These three factors most directly impact your ability to deliver safe, expanding services while maintaining regulatory compliance across your coverage areas. Pricing matters, but alignment and accessibility matter more. You're investing in predictability and mentorship, not the lowest monthly fee.
Cost Reality Check: Paying for Outcomes, Not a Signature
The market offers "signature-only" arrangements at minimal cost. These typically provide nothing beyond required documentation—no chart review, no accessible guidance, no mentorship. When state boards conduct audits or when complex clinical questions arise, that bargain arrangement becomes a liability.
Quality collaboration operates as a retainer-based partnership, not a transaction. The investment—which practitioners commonly report ranging from $500 to $1,250 monthly depending on practice complexity, specialty, and state requirements—funds ongoing access, systematic chart review, and genuine clinical support. This isn't overhead. It's infrastructure that enables growth.
For NPs still evaluating the financial and legal risks of informal arrangements, the key distinction comes down to audit resilience and operational functionality. Can the collaboration withstand regulatory scrutiny? Does it genuinely support clinical decision-making? If the answer to either question is uncertain, the arrangement isn't truly protecting the practice.
"Compliance keeps the doors open; collaboration blows the roof off your potential."
State Fit and Scalability
Collaboration requirements vary significantly across the country. The AANP State Practice Environment map classifies states as full practice, reduced, or restricted, with each category carrying different collaboration mandates. Some states require in-state licensure for collaborating physicians. Others accept out-of-state collaborators if the NP practices in person. Telehealth adds another layer of complexity: patient location during the visit typically determines which state's regulatory requirements apply, not provider location.
Consider a few common scenarios. An NP practicing exclusively in New York must work with a physician who understands that New York State regulations require written practice agreements or collaborative relationships, particularly for practitioners at certain experience levels. The collaboration agreement must align with state board expectations and document appropriate oversight mechanisms.
For practices operating across New Jersey, New York, and Pennsylvania, the challenge multiplies. Each state has distinct requirements for how collaboration is documented and maintained. Building a relationship with a physician—or a coordinated physician team—licensed in all target states prevents constant disruption and ensures consistent oversight quality.
Telehealth practices face perhaps the most complex landscape. In most regulatory frameworks, the patient's physical location during the visit determines which state's rules govern the encounter. Planning multi-state telehealth expansion without proper licensure alignment and regulatory understanding quietly creates compliance gaps that surface only when problems arise.
This complexity makes state-matched collaboration essential for both compliance and growth. For practices with expansion plans, evaluate whether your collaboration structure scales. Adding new states, services, or delivery models should enhance your partnership, not require starting over with new physicians.
Your Choices and Common Traps
The marketplace presents roughly three collaboration models. Understanding each model's limitations helps clarify what quality partnership actually requires.
The "Signature-Only" Approach: Low cost. Minimal involvement. Maximum risk. These arrangements often fail to document sufficient oversight during audits. When clinical questions arise, there's no accessible support. The relationship typically provides a signed form and little else—no regular chart review, no systematic feedback, no availability for guidance. During board inquiries, explaining that "we barely communicated" creates significant vulnerability. The initial savings evaporate when regulatory or clinical problems surface.
The Employee Medical Director Model: Some large practices hire full-time or part-time medical directors as employees. This creates substantial overhead: salary, benefits, practice liability exposure, management complexity. For small to mid-size independent practices, this model often feels financially prohibitive. It's designed for multi-site systems with dozens of providers, not solo practitioners or small teams. A fractional, retainer-based collaborator provides strategic oversight without the employment burden.
The Strategic Partner Model: Board-certified physicians in Internal Medicine, Family Medicine, Emergency Medicine, and Psychiatry with over 10 years of collaboration experience, offering systematic chart review, accessible communication during business hours, and mentorship-oriented guidance. This is the model that serves most independent NPs effectively: professional support without employment overhead, genuine clinical accessibility without full-time costs, and specialty alignment that enables practice growth rather than simply satisfying minimum requirements.
The trap many practitioners fall into is prioritizing speed over certainty. A "fast match" sounds appealing when launching or expanding. But if that match lacks specialty alignment, reliable availability, or genuine mentorship capacity, the convenience disappears quickly. Taking time to find the right partner pays dividends for years.
How Working with Physician Collaborators Looks in Practice
From initial contact to steady collaboration rhythm, the process is designed for speed, predictability, and minimal administrative friction. Here's what a typical engagement timeline looks like:
Week 0: Initial Consultation and Quote
You share essential information about your practice: your degree, states where you serve patients, current malpractice coverage status, practice type (general medicine, behavioral health, telemedicine, urgent care, infusion therapy, integrative medicine, or med spa), whether you prescribe controlled substances, your NPI number, and key details about your clinical focus and growth plans. Based on this profile, you receive a realistic price band and match timeline. Many NPs are matched with an appropriate collaborating physician within one week.
Week 1: Match and Onboarding
You're introduced to a board-certified physician whose specialty and state licensure align with your practice needs. Together, you review expectations: how the chart review process works, how often you'll connect for guidance, and how to reach them during business hours. Communication protocols are established—when to text or email for routine questions, when to schedule Zoom consultations for more complex discussions, and what constitutes an appropriate escalation.
Weeks 2-4: First Chart Review and Working Relationship
A sample of your charts undergoes review with written feedback. You have a call or Zoom session to discuss themes, refine existing protocols, and explore opportunities for service expansion. This initial review establishes the quality baseline and helps both parties calibrate expectations around documentation standards, clinical decision-making, and growth opportunities.
Ongoing: Steady Rhythm and Clear Escalation Paths
The relationship settles into a predictable cadence. You know when to use text or email for quick questions, when to schedule a Zoom consultation for complex cases, and what response times to expect during business hours. As your practice grows or adds states, the collaboration structure scales with you. The monthly retainer model ensures consistent access without per-question billing or access restrictions.
For specific questions about communication methods, timeline expectations, or pricing structures, the frequently asked questions provide detailed guidance. For state-specific regulatory considerations, dedicated pages for New York, New Jersey, and Pennsylvania outline regional requirements and collaboration approaches.
Turn Collaboration Into a Growth Lever
The distinction between compliance and growth sits in how you frame the collaboration requirement. If it's merely a signature securing your ability to practice, you're meeting the minimum. If it's a strategic partnership with specialty-aligned guidance, accessible mentorship, and systematic oversight, you're building infrastructure for sustainable expansion.
Review the Growth Partner Evaluation Matrix above and score your current collaboration—or use it to evaluate potential new partnerships. Confirm that your target states appear on the states we cover page. Then request a free quote or book a free consultation to discuss your practice type, growth goals, and timeline.
From there, you'll have clarity on what a specialty-matched, growth-oriented collaborating physician could deliver over the next 12 to 24 months—not just for your compliance documentation, but for your clinical confidence, operational stability, and revenue trajectory.
Our Editorial Process:We prioritize state statutes, state board guidance, NCSBN resources, and HHS materials. Every statement that could affect compliance is checked against authority sources and dated. We avoid vendor/competitor sources for definitions and requirements. Articles receive a legal/compliance pass for clarity before publication.
About the Physician Collaborators Insights Team
The Physician Collaborators Insights Team is our dedicated engine for synthesizing complex topics into clear, helpful guides. While our content is thoroughly reviewed for clarity and accuracy, it is for informational purposes and should not replace professional advice.
Disclaimer: This guide is intended as a comprehensive starting point. For decisions specific to your unique situation, we always recommend consulting a qualified professional.